Over The Crest
Sharpening the Edge: Bringing Precision to Psychiatry
Psychiatry has long advanced through persistence and experimentation. Now, precision psychiatry sharpens the approach bringing clarity, efficiency, and renewed hope to millions.
Modern psychiatry, for all its life-changing contributions, remains fundamentally imprecise. Clinical decisions are often guided by a “one-size-fits-most” model that is blind to the severe biological diversity of mental illnesses, leaving both clinicians and patients struggling to find a sufficient treatment [1]. This results in part from the lack of an easily performed, and most importantly, accurate, biomarker test as is common for many medical diseases. The consequences are profound: patients cycle through treatments for months or years, experiencing delayed recoveries, worsening symptoms, and sometimes devastating side effects [1].
Psychiatric treatment today can be broad and blunt. Pharmacotherapy remains the first-line approach, with antidepressants, antipsychotics, and mood stabilizers prescribed based on symptom clusters. However, the effectiveness of this strategy leaves something to be desired: only about 33% of patients achieve remission with their first antidepressant [1]. Most are subject to prolonged trial and error periods, each failure broadening their risk of worsening symptoms and side effects. In many cases, patients are not just battling their original disorder but incurring new complications from these periods.
Psychotherapies can be valuable alternatives but their effectiveness varies significantly across patient populations. Neuromodulation techniques like transcranial magnetic stimulation (TMS) and electroconvulsive therapy (ECT) show efficacy for treatment-resistant depression, but their costs and access barriers are substantial.
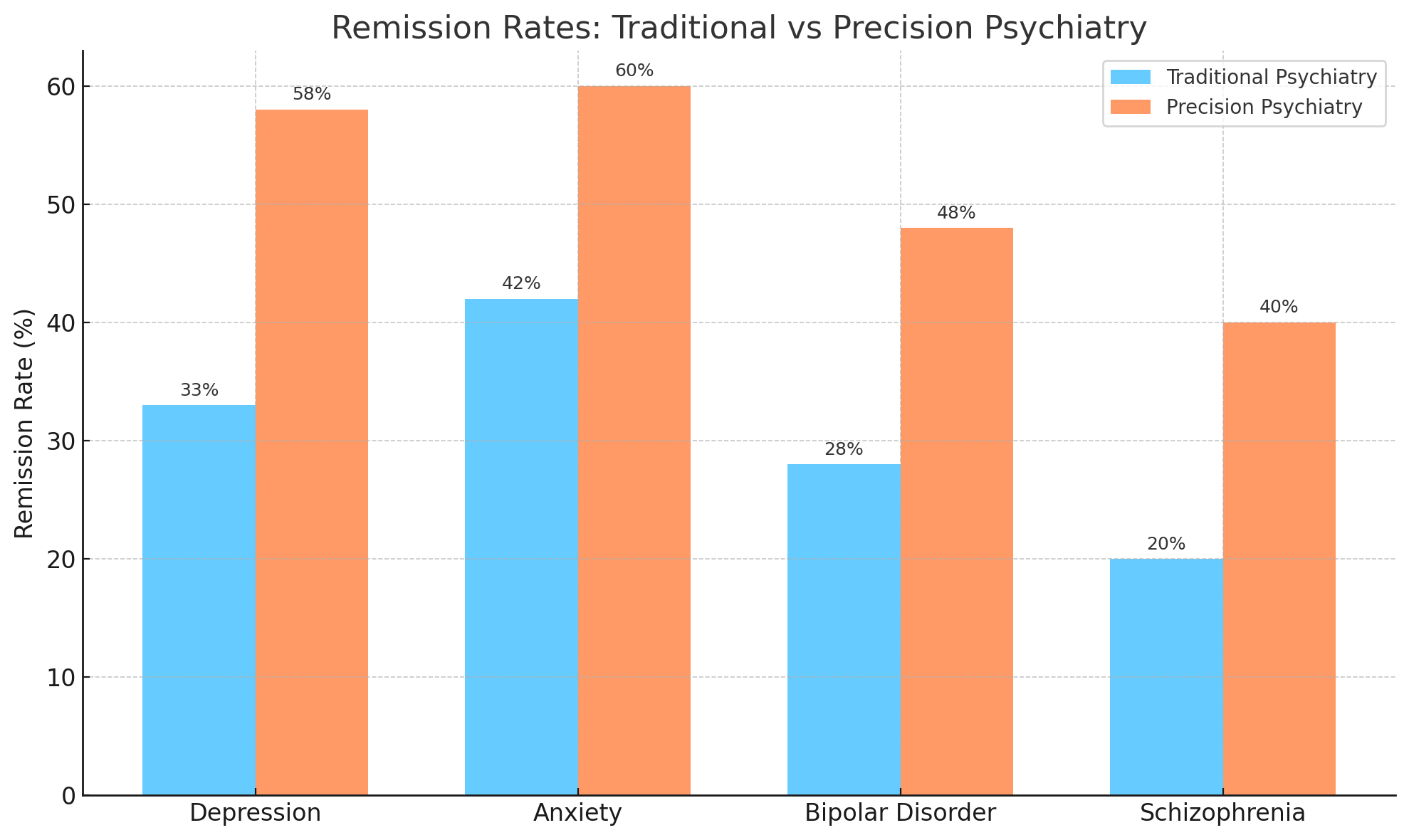
Source: Castro Crest, 2025. Traditional psychiatry refers to standard clinical practices based on symptom-driven diagnosis and trial-and-error treatment selection, typically without biological markers. Precision psychiatry refers to emerging approaches that leverage biological, genetic, inflammatory, or digital biomarkers to match patients with treatments most likely to succeed based on individual characteristics. Data reflects published remission rates from landmark studies (e.g., STAR*D) and early precision psychiatry trials.
The inefficiency of this system yields an extraordinary price, both monetarily and socially. Mental health conditions cost the U.S. approximately $282 billion per year [2], a figure projected to accelerate without change. Globally, the failure to address mental health is expected to add an additional $14 trillion to the world’s economic burden by 2040 [3]. Beyond just dollar amounts, these figures represent lives derailed, systems overwhelmed, and opportunities lost. More specifically, these clinical realities drive direct and indirect healthcare costs. Every ineffective treatment cycle generates new physician visits, hospitalizations, medication switches, secondary psychological complications and comorbid medical conditions. Indirect costs of lost income, long-term disability, and early mortality all amplify the burden. Mental illness reduces personal consumption by 6.2% for mild cases and by 13.9% for serious mental illness [2].
The current model, statistically speaking, is more likely to fail than succeed. However, precision psychiatry introduces a potentially radical shift in efficacy by treating the individual, not the diagnostic category. Utilizing a growing range of emerging biological measures including genomic data, inflammatory biomarkers, digital phenotyping, and neuroimaging, precision psychiatry is a realistic goal that aims to predict individualized treatment outcomes rather than relying on population averages.
Instead of cycling through medications via trial and error, clinicians could use biological and digital markers to identify the most effective therapy on the first attempt. This is already being accomplished with measurement of specific enzymatic serotypes in individuals that guide physician prescriptions for psychiatric disorders. Indeed, early studies suggest this approach could lift remission rates from 33% to over 50% in depression by targeting treatments more precisely [4].
In essence, precision psychiatry replaces the blunt instrument of current care with a scalpel by delivering faster recoveries, fewer side effects, and more durable outcomes, all in fewer attempts.
Precision psychiatry directly addresses three massive gaps. First is the clinical gap. Psychiatry today struggles with prediction. Treatments are largely agnostic to underlying biological variability. Precision psychiatry would offer outcome forecasting at the individual level, dramatically reducing trial-and-error prescribing.
Second is the public health gap. Faster and more accurate interventions reduce emergency room admissions, lower disability rates, lower disability rates, reduce associated outcomes such as crime and substance abuse, and decrease long-term reliance on social services. All of these downstream improved treatment effects could increase national consumption by 0.7%, equivalent to $78 billion annually in the United States [2].
Third, and perhaps the most striking, is the economic gap. Globally, untreated or ineffectively treated mental illness threatens to add $14 trillion in costs by 2040 [3]. A system that can intervene earlier and more accurately could shift psychiatric care from a chronic financial liability into a growth sector. Nationally and internationally, faster recoveries and fewer relapses could unleash productivity gains, reduce healthcare burdens, and improve societal resilience.
If precision psychiatry succeeds, faster remissions will lower direct healthcare costs, avoiding treatment-resistant goose chases. Care resources for both the patient and provider will be conserved with targeted interventions that reduce spending on secondary health issues driven by medication side effects. The NBER model shows that even a modest 10% improvement in mental health treatment efficacy could yield $78 billion per year in additional U.S. consumption [2].
For insurers, employers, healthcare systems, and governments, the value proposition is clear: precision psychiatry is not just better care, it is a smarter investment, assuming it succeeds.
In summary, the unmet needs in psychiatric treatment today are critical, both financially and socially. While behavioral health investment is already trending toward a $400 billion global market [6], precision psychiatry remains dramatically undercapitalized. Current precision-focused startups represent less than 5% of mental health venture funding [5], signaling substantial white space for early movers. This is not a crowded marketplace—it is a sector waiting for category-defining winners.
Early validation exists. In late 2023, Bristol Myers Squibb acquired Karuna Therapeutics—a company developing a precision-targeted schizophrenia treatment—for $14 billion, sending a strong signal that pharma is willing to pay premium multiples for validated neuropsychiatric precision assets.
The exit pathways are clear. Acquisition by major pharmaceutical companies seeking differentiated CNS pipelines, strategic partnerships with insurers eager to reduce psychiatric treatment costs, and public market listings, following proof of clinical scalability are all viable outcomes to liquidity and impact.
The market conditions today resemble early precision oncology: massive unmet need, growing data infrastructure, and initial proof points, but with no dominant players yet. For venture capitalists, this presents the rarest kind of opportunity: a massive addressable market, enormous inefficiency demanding solutions, early technological inflection, and minimal entrenched competition.
_____________
References
[1] STARD Trial: Rush, A. J., et al. (2006). Acute and Longer-Term Outcomes in Depressed Outpatients Requiring One or Several Treatment Steps: A STARD Report. American Journal of Psychiatry.
[2] Werning, I., Zhao, S., & Zhang, D. (2024). The Macroeconomics of Mental Health. NBER Working Paper 32354.
[3] Deloitte Insights. (2024). The Economic Burden of Mental Health Inequities.
[4] Precision Psychiatry Market Size. (2024). StraitsResearch: Precision Psychiatry Market Analysis.
[5] PitchBook Data Inc. (2024). Mental Health Venture Funding Database.
[6] Towards Healthcare. (2024). U.S. Behavioral Health Market Size, Share & Trends Analysis Report. Retrieved from https://www.towardshealthcare.com/insights/us-behavioral-health-market